
|

|

|

|
|
Archives of Physical Medicine and Rehabilitation,
1991;72:734-7
Trigger Point of the Posterior Iliac Crest:
Painful iliolumbar ligament insertion
or cutaneous dorsal ramus pain?
An anatomic study
Jean-Yves Maigne, MD, Robert Maigne, MD, Physical Medicine, Hotel-Dieu
Hospital, 75181 Paris Cedex 04, France |
Abstract. A trigger
point is frequently found over the iliac crest at 7 to 8cm from the midline
in low back pain syndromes. Previously, this was described as either a
painful insertion site of the iliolumbar ligament or pain in the
distribution of the cutaneous dorsal ramus of the first or second lumbar
nerve. The authors performed 37 dissections, and they report their anatomic
findings. The iliac insertion of the iliolumbar ligament is inaccessible to
palpation, being shielded by the iliac crest. The dorsal rami of LI or L2
nerve roots, however, cross the crest at 7cm from the midline, and this
distance closely correlates with the dorsal projection of the iliolumbar
ligament insertion. These rami are superficial and dorsal to the crest,
easily accessible to palpation. In two of the 37 dissections performed, some
rami were found to be narrowed as they crossed through an osteofibrous
orifice over the crest, thus being susceptible to an entrapment neuropathy.
The authors conclude that the trigger point sometimes localized over the
iliac crest at 7cm from the midline likely corresponds to elicited pain from
a cutaneous dorsal ramus originating from the thoracolumbar junction rather
than from the iliac insertion of the iliolumbar ligament.
Low back pain is a common syndrome with various etiologies. In some cases,
examination of soft tissues reveals the presence of trigger points, defined
as points of maximal tenderness, where pressure reproduces actual pain.
These points may correspond to underlying muscles, tendons, ligaments, or
nerves in conjunction with their location.
Two particular notions have attracted our interest; they are the rather
precise position of one of these points and its frequent occurrence. The
iliac trigger point is situated over the iliac crest, at 7 or 8 cm from the
midline (fig 1). It can be associated with other trigger points, as in the
case of fibromyalgia. It can also be unique and unilateral in patients
suffering from non radiating, ipsilateral low back pain. These patients
present with normal neurologic examination, absence of tension signs, and
normal lumbosacral and pelvic roentgenograms. Two syndromes have been
proposed to regroup and explain the significance of this trigger point: the
iliolumbar syndrome and the thoracolumbar junction facet syndrome.
The iliolumbar syndrome as described by Hackett (1) and by Hirschberg and
associates (2) is characterized by posterior, unilateral iliac crest pain.
Other symptoms include referral of pain into the groin or the lateral aspect
of the hip and aggravation of the pain by contralateral bending. However,
the best clinical sign is unilateral tenderness upon focal palpation over
the posterior iliac crest on the involved side. This trigger point is
thought to correspond to the insertion of the iliolumbar ligament.
Anesthetic infiltration of this point abolishes all signs and symptoms, thus
establishing the diagnosis of an "iliolumbar syndrome."
The facet syndrome previously describedd is characterized by (a) a focal,
painful area in the dermatome of corresponding cutaneous dorsal rami (T12,
LI), maximal at the posterior iliac crest, (b) palpation along the crest
revealing a trigger point that would correspond to the emergence of this
nerve and pressure at this point readily reproducing or aggravating the
patient's symptoms, and (c) confirmation of a painful facet joint at the
thoracolumbar junction when local pain is readily reproduced by
posteroanterior pressure over the facet joint in question. Anesthetic
infiltration around the involved joint relieves the low back pain and also
suppresses this trigger point.
Thus, it can be seen that posterior iliac crest tenderness may correspond
either to the insertion of the iliolumbar ligament or to the cutaneous
dorsal rami that cross the posterior iliac crest and originate at the
thoracolumbar junction. An anatomic study was undertaken to clarify the true
origin of this point over the posterior iliac crest, and to identify the
structures that are accessible to palpation during routine clinical
examination.
Thirty-seven adult cadavers (24 male and 13 female) were dissected to
examine the
iliolumbar ligament and the cutaneous
branches of the dorsal rami from T11 to L3. Special attention was paid
to the ligamentous insertion at the crest as well as to the dorsal rami as
they crossed this site. Initially, the thoracolumbar fascia was cut along
its medial insertion, exposing the nerves. The nerves were then dissected
proximally to the intervertebral foramen to identify the level of origin and
distally as far as their finest ramification would allow; a binocular lens
was used when necessary.
Fig 1: Iliac crest trigger
point, located 7 to 8 cm from the midline, is a frequent finding in low back
pain patients.
Fig 2:
Posterior view of the right iliac crest. The iliolumbar ligament runs from
the transverse process of L5 (T) to the ventral margin of the crest (V).
Only the dorsal margin (D) of the crest is accessible to palpation.
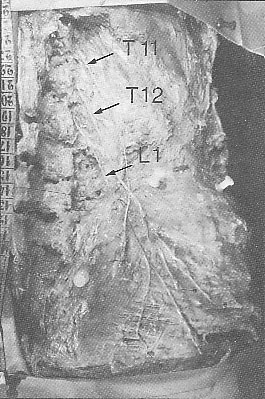 Fig
3: Right side. The needles indicate
the line of the iliac crest. The course of the cutaneous dorsal rami of T11,
T12, and L1 are shown; L1 is the last lumbar cutaneous ramus. Note the
unusual disposition as T11 crosses over T12 and L1. Fig
3: Right side. The needles indicate
the line of the iliac crest. The course of the cutaneous dorsal rami of T11,
T12, and L1 are shown; L1 is the last lumbar cutaneous ramus. Note the
unusual disposition as T11 crosses over T12 and L1.
The iliolumbar ligament originated from the transverse process of L5 and
inserted deep into the ventral margin of the iliac crest, 6 to 7cm from the
midline. The insertion was shielded by the crest dorsally, making it
inaccessible to palpation (fig 2). Our dissection showed that the crest was
usually crossed by two or three dorsal rami that innervated the cutaneous
layers of the buttock (fig 3). Futhermore, there were anatomic variations in
that Ll was the most medial nerve in 22 of 37 dissections; whereas, L2 was
the most medial in the remaining 15 cases. It was also noted that the L2
nerve occasionally received anastomosis from L3, although this relationship
was not constant. The most lateral nerve was usually T12 (28 of 37
dissections), with L1 comprising the rest (nine of 37). However, as the
medial and lateral branches crossed the crest, the distance between them
varied from 1 to 5cm (fig 4). Of particular interest was the finding that
the medial nerve (L1 or L2) became superficial by passing over the crest
through an osteofibrous orifice consisting of the thoracolumbar fascia and
the superior rim of the iliac crest (fig 5). This osteofibrous orifice was a
rigid structure that, in two instances, was seen to severely compress the
nerve (fig 6).
Fig 4:
The position
of the dorsal rami at the iliac crest. The dissections showed three main
patterns: type 1 was the most frequent (22 of 37), with T12 lateral, M
medial, and L2 absent; in type 2, L2 is medial and the lateral nerve is
either M (type 2a, five cases) or T12 (type 2b, five cases); and in Type 3,
L2 received anastomosis from L3, up or down the crest. The lateral nerve was
M (type 3a, four cases) or T12 (type 3b, one case). Note the constant
distance (7 to 8 cm) separating the nerve from the midline as it crosses the
crest.
Fig 5:
The medial cutaneous dorsal ramus crosses the iliac crest by
passing through a rigid osteofibrous orifice (arrow). The superior aspect of
this orifice consists of the thoracolumbar fascia (TFL), and the inferior
aspect of the superior rim of the iliac crest (small dots).
Fig 6:
In two instances the medial branch was compressed by an
osteofibrous orifice, possibly representing, in our view, an entrapment
neuropathy.
In a postmortem study such as this, special care must be taken when
combining the results with clinical evidence. Bearing this in mind, the
following conclusions are advanced.
In our 37 dissections,
the iliolumbar ligament insertion was always located on the ventral aspect
of the crest. Similar observations were made by Luk and colleagues, who
noticed that the ligament blended with the periosteum of the ventral margin
of the iliac crest, and by Gray, who said the insertion of the ligament was
on the crest in front of the sacroiliac joint. This leads us to think that
the iliolumbar ligament insertion is
inaccessible to palpation, since it is shielded by the crest. Consequently,
the trigger point over the iliac crest, located 7 to 8cm from the midline
could not correspond to the ligament's attachment.
However, this distance did clearly correspond to the position of the medial
cutaneous dorsal rami (L1 or L2) as it crossed the crest superficially on
its dorsal aspect. At this site, the nerve was always accessible to
palpation as it passed dorsally to the crest, having become superficial by
perforating the thoracolumbar fascia through a rigid osteomembranous
orifice. The nature of this orifice leaves the nerve prone to irritation or
compression.
 Conclusion Conclusion
Thus, this anatomic study allows us to think that a clinically reproducible
trigger point, situated at the level of the iliac crest and 7 to 8cm from
the medial line, likely corresponds to the presence of a nerve (and not to a
ligamentous insertion) that can be compressed against the iliac crest during
palpation. This nerve could produce pain, either by referral from a facet
syndrome or secondary to local compression or irritation
Acknowledgment: We would like to thank Dr. Charles Molta, MD,
for his assistance in the preparation of this paper.
References
1. Hackett GS. Ligament and tendon relaxation (skeletal disability) treated
by prolotherapy (fibro-osseous proliferation). 3rd ed.
Springfield IL: Thomas, 1958.
2. Hirschberg GG, Froetscher L, Naeim F. Iliolumbar syndrome as a common
cause of low back pain: diagnosis and prognosis. Arch Phys Med Rehabil
1979;60:415-9.
3. Maigne R. Low back pain of thoracolumbar origin. Arch Phys Med Rehabil
1980;61:389-95.
4. Luk KDK, Ho HC, Leong JCY. The iliolumbar ligament: a study of its
anatomy, development and clinical significance.
J Bone Joint
Surg [Br] 1986;68:197-200.
5. Gray H. Gray's anatomy. 35th ed. Philadelphia: Saunders, 1973:414.
|
|

|
|

|

|
|
|

|
|
